Burnout: Part 4: Resolving the Controversy
Hello again:
Thanks for staying tuned for Part 4, as this subject is important and lends an understanding as to how chronic health conditions evolve and what to do about them…so this newsletter is a bit longer than usual.
If you have not read this link, please do so to understand the issues, it is not that long and is pretty good:
From this article: “A recent review of 58 studies concluded that there is no scientific basis to associate adrenal impairment as a cause of fatigue. The cortisol level, when checked four times in a 24-hour period, was no different between fatigued and healthy patients in 61.5% of the studies…. In summary, there is no formal criteria to define and diagnose adrenal fatigue.”
However, repeatedly and commonly on labs, it can be observed that there are states of adrenal function that are not normal, but not Cushing’s or Addison’s. This is where you can see changes in adrenal function that are not pathologically based. An example would be high morning cortisol, that trends to normal the rest of the day. Or a normal morning cortisol, that drops low during the day but goes up too high at night. Another example is that cortisol is a low normal all day. Currently within allopathic medicine, the term adrenal fatigue is not a recognized condition until the cortisol production becomes too low, then this is called adrenal insufficiency.
Additionally, within functional medicine concepts, adrenal fatigue can be the state that precedes insufficiency that is not brought on by an autoimmune disorder or hypothalamic-pituitary failure but the KEY is that adrenal dysfunction can be a result of chronic stress that stems from mental/emotional stress, nutritional stress, chronic illness of any type, autoimmune conditions, latent or hidden infections, poor food choices, lack of sleep or a combination of all types of stress facing any individual. This type of disorder IS recognized within standard medicine (see below).
How do we reconcile these observations?
First of all, this study seems to assume that adrenal issues are part of all fatigue states, yet it is widely recognized that fatigue often/usually has MULTIPLE causes. Even the Harvard blog mentions that. So, there is no reason to make the broad assumption that all fatigue/burnout states have adrenal dysfunction at the root of the fatigue. Indeed, in the above referenced study, there were 38.5% of the patients that may have met the criteria for adrenal fatigue. Why were those individuals not explained, in other words, if 38.5% of the cases had some form of match up to adrenal fatigue, why not investigate that and come up with criteria and definitions? Perhaps adrenal fatigue affects every 2 out of 5 cases of fatigue or burnout and it is not an all or nothing case. Or maybe this is part of HPA axis dysregulation (see below).
Secondly, there are other organs that are recognized that become fatigued, such as the pancreas, kidneys, heart, brain and even joints…why not the adrenals in some cases?
Thirdly, it depends on how you read lab tests, and that means, are you looking for pathology (Cushing’s and Addison’s) or for disturbances of function (adrenal fatigue). It simply can be a matter of gradation that does not fit the standard way of looking at lab results. Standard evaluations have a range of normal, and ANYTHING in the normal range is usually considered Ok, even if the patient has symptoms. In other words, it is a Black or White situation, there is no room for Grey. This way of looking at things has been enormously useful and has greatly benefited humanity. However, when it comes to chronic, multi-system health issues where no clear pathology can be found in the usual way of looking at lab results, it is often useful to look at lab tests where you narrow the normal range (which can be called an Optimal range) and those numbers that are not Optimal but not Black, can be considered to be Grey.
The Grey zone is where there is a lack of normal function that precedes pathology and is often called a disturbance of FUNCTION as opposed to pathology. In Grey zone issues, there are usually no prescription medications or standard treatments recognized…in other words, if you do not have a tool for it, you may not look for it, therefore it may not be considered to be real or exist. This may apply to adrenal fatigue, which is not a disease but a functional condition, and for the most part, functional (Grey zone) conditions often respond best to comprehensive natural supportive therapies, which the author kindly acknowledges when he states: “Alternative and complementary clinicians often have better results, because the appointments tend to last longer and they view patients through a more holistic lens.” The functional medicine approach tends to look at multi-system interconnectedness and seek to support and balance those dysfunctional relationships, and certainly acknowledges, respects, recommends and employs standard methods right alongside functional measures to assist and support optimization. In other words, in my opinion, there is no controversy, but there are two distinct conditions supported by clinical observations and they are Black (Addison’s & Cushing’s) and Grey (adrenal fatigue or over-activity).
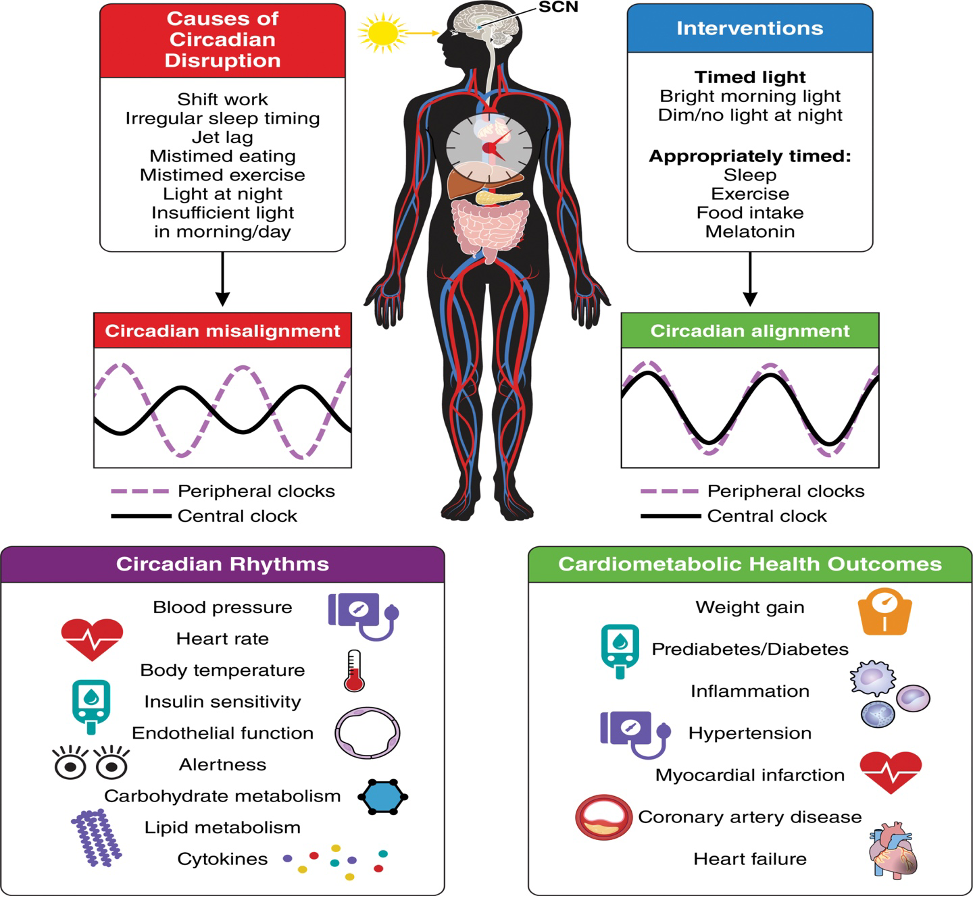
Lastly, and most likely, what we are all really looking at is HPA axis dysfunction or dysregulation, which means that adrenal fatigue states should be viewed from this perspective and as a part of a larger issue. This means that adrenal supplements ALONE will seldom get the results we would all like to see. This makes sense of the abnormal cortisol lab tests that we see even when there is no adrenal or pituitary pathology such as seen in Cushing’s and Addison’s.
Bottom Line: If you are having unreasonable fatigue, any type of chronic condition(s) or the symptoms that were listed in the previous newsletters, part of the investigation should include a morning cortisol test. If that is high or low, then depending of the results, it may be prudent to follow up with a salivary cortisol rhythm test. We often run these lab tests, and the vast majority of the time, we find functional problems, and rarely find pathologically low or high cortisol that requires the immediate referral to an endocrinologist.
HINT: It is usually more important and useful to find the underlying causes of the ongoing stress response that led to the overactive state (high cortisol), then later the crashed state (low cortisol) than it is to simply support adrenal function by itself. This is why the scientific literature DOES recognize HPA dysregulation or dysfunction as a real entity:
In the next newsletters, we will go over HPA axis dysregulation and it’s causes, then self-care methods relating to functional disturbances in the HPA axis that include nutrition, stress reduction and lifestyle support for elevated morning cortisol or low cortisol patterns and why I seldom use adrenal supplement protocols.
The post Burnout: Part 4: Resolving the Controversy appeared first on RICHMOND CHIROPRACTIC NEUROLOGY.